Make an Appointment
Injuries caused by falls are one of the leading causes of morbidity and mortality in Australia for our older generations. They’re the leading cause of hospitalisations for Australians over 65 years old.
Of these falls that end up in hospitalisation, 3.6% result in death. Additionally, 30% of these victims will die within six months. Falls are also one of the major contributing factors to RACF admissions.
Definition of Fall?
According to the World Health Organisation,
“a fall in an event which results in a person coming to rest inadvertently on the ground or floor or other lower level.”
What categorises a fall is that a fall is involuntary as opposed to a person’s behaviour that led to them putting themselves on the floor.
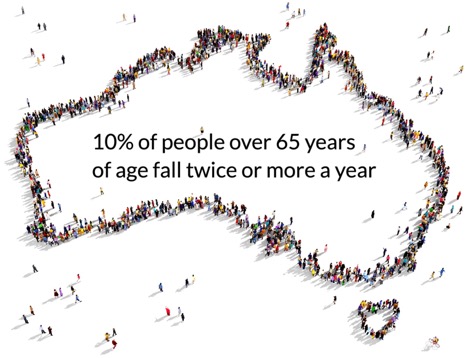
Current Incidence in Australia?
Even though a fall might seem like an inconsequential occurrence for younger folks, it’s clearly a big deal in the older generation.
In Australia, 10% of people over 65 years of age fall twice or more a year. If you’re over 80 years old, the likelihood that you’ll fall every year increases to 80%. For those over 75 years old, 56% of all hospitalisation will have been due to falls
In 1998, falls resulted in 1,000 deaths and 50,000 hospitalisations. These are huge numbers and require a real preventative effort in aged care.
Hospitalisations in Australia?
Hospitalisations due to falls of older people in Australia don’t seem to be declining anytime soon. The numbers are as high as ever and might even be increasing.
Between 2009 and 2010, it was estimated that 83,800 hospitalisations of people over the age of 65 were due to falls, up 5,100 cases from the previous year.
The number of hospitalised injury cases rose from 327,000 in 1999–00 to 480,000 in 2014–15,’ said spokesperson Professor James Harrison from the AIHW's National Injury Surveillance Unit, based at Flinders University.
‘This equated to 1 person requiring hospitalisation in every 58 Australians in 1999–00, rising to about 1 in 50 in 2014–15’.

One-third of these falls resulted in an injury to the hip and thigh with most resulting in a hip fracture. Head injuries accounted for 1 in 5 hospitalised cases and were more common for men than women.
Among all age groups, women accounted for most of the fall-related hospitalisations. The rate of hospitalised fall injuries involving older women exceeded 3,000 out of 100,000 people.
The most common causes of these hospitalised falls were slipping, tripping, and stumbling with 70% occurring either at home or an aged care facility.
Unfortunately, some of this data is unclear, but common areas in the home for falls to take place were outdoor areas, bathrooms, and bedrooms while 48% of these hospitalised falls took place in “other and unspecified places” in the home.
As for the burden placed on hospitals due to these falls, one in every ten days that a person over 65 spent at a hospital was attributed to an injurious fall with the total length of stay per fall injury case is estimated at 15.5 days.
About 10,000 of these fall cases had been transferred to another hospital, adding 0.14 million patient days to that total. Plus, that doesn’t even cover follow-up care.
Fall-related follow-up hospitalisations numbered almost 34,000, accounting for a further 0.57 million patient days.
Research?
According to research, the hip and thigh is the most likely area to sustain an injury as a result of a fall. In fact, 91% of hip fractures are caused by falls and is the most common reason for hospitalisation from falls.
Wrist fractures are also a common fall-related injury as people attempted to break their fall by putting out a hand.
Consequences of Falls?
Let’s take a look at all the potential consequences of falls.
First of all, there’s a risk of fractures which we’ve already mentioned. Hip fractures and other fractures are a huge consequence of falls for the older generation.

Even if one doesn’t fracture a bone, they’re still likely to suffer skin tears, bruising, and hospital admission. Plus, it does deeper damage in a mental capacity.
Falls often lead to a loss of confidence which turns into increased disability and increased dependence. Plus, caregiver stress and fear of litigation among clinical and administrative staff only add to the issue.
Risk Factors?
The first step in preventing a problem is to understand the risk factors. These risk factors can either be intrinsic (personal) or extrinsic (environmental).
Common intrinsic risk factors for falls among the older generation include:
- Chronic diseases: OA/RA, Diabetes, Parkinson’s, MS, HT, CVD, COPDs, Dementia
- Behaviours: confusion, agitation, wandering, impulsive, fidgeting
- Aging: causes decreased strength, balance, and reaction time
- History of falls: four or more falls in the last year equates to an increased risk for falls
- Cognitive impairment: Presence of cognitive disorders, Dementia, Alzheimer’s, STML, delirium
- Footwear: ill-fitting footwear or using footwear such as slippers, thongs, and socks
- Continence: 2/3 of residents at RACFs experience urinary or fecal incontinence that is not part of the normal aging process
- Medications: sedatives, antidepressants, antipsychotics, antihypertensive medications, diuretics, NSAIDs, vasodilators; all of which can cause side effects including hypotension, drowsiness, confusion, dizziness, blurred vision, and delirium
- Vision and hearing deficits: Glaucoma, Cataracts, Macular degeneration
- Unsteady gait: related to aging
- Decreased strength and balance: related to aging
- Acute health conditions: UTIs, TIAs, delirium, dehydration, constipation, post-anesthetic
Conversely, common extrinsic risk factors for falls among the older generation include:
- Lighting: poor lighting
- Height of bed, chairs, or toilets: too high or too low
- Clutter: dangly wires, furniture, and equipment
- Walking aids: old, worn out, or inappropriate
How to and Who Can Prevent Falls?
The people in aged care facilities best suited to prevent falls are pretty much everyone there. It should be managers, doctors, AINs, RNs, EENs, RAOs, cleaning staff, residents, maintenance staff, kitchen staff, clerical staff, resident’s families, visitors, laundry staff, care managers, and PTAs.
The best practices for preventing falls includes four components.
- Implement standard prevention strategies (i.e. exercise, physiotherapy)
- Identify falls risks
- Address identified falls risks
- Prevent injuries
In order to prevent falls, it’s important to get educated on a few key factors.
Fight Age?
Fighting age means working to slow down its effects. This could mean promoting mobility and activity like walking and exercise. Balance and weight-bearing exercises are essential. You might also encourage participation/independence in ADLs.
Simply two days of exercise per week with an instructor for at least 75 minutes over the course of a year has shown the most benefit.
A 2003 study by Becker claimed that
“supervised, group-based progressive balance and resistance exercises using ankles weights and dumbbells plus hip protectors, environmental modifications, gait aid checks, and education all showed a significant reduction in falls.”
Yet, even though group exercise is a great activity option to offer residents, in fact, individual exercise and walking with caretakers is essential as well.
Managing Residents’ Change in Condition?
When it comes to managing residents’ change in condition we’re referring to a few things.
Firstly, it’s providing the support needed for safe transfers and mobility by ensuring a walking aid or proper footwear.
It’s also about ensuring staff are following the Manual Handling Plans, any changes are being reported to the RNs for investigation, you’re encouraging hip protector compliance, and you’re reporting maintenance needs for equipment.
Lifestyle?
Pay attention to the lifestyle of your aged facility residents to help prevent falls.
You can do this by ensuring adequate hydration and a balanced diet with calcium, auditing and adapting the environment, creating a dynamic RAO programme that occupies the residents' time in a meaningful way, allow residents to rest when tired but otherwise encourage wakefulness throughout the day, and adhering to the toileting programs.
Environmental Adaptations?
Adapting the environment is an important step in removing some of the extrinsic causes of falls which can include:
- Decreasing clutter
- Providing adaptive devices
- Ensuring good lighting
- Ensuring appropriate height of bed and chairs
- Ensuring appropriate walking aides to those who need them
The walking aides you should be familiar with are rollator frames (RF), pick-up frames (PUF), Canadian (C/C), auxiliary (A/C), forearm support frame (FASF), walking sticks, and quad sticks (QS).
Involving Residents?
Creating a supportive community surrounding issues with falls is one of the best ways to prevent falls in the first place. Many people actually become afraid to talk about having a fall since they feel it means they will lose their independence.
When it comes to health care, consumer participation is central to making sure it’s of high quality and maintains its accountability. Falls prevention could be unfamiliar and difficult to understand for many residents so it’s important to convey the message that talking about their falls actually will help them stay independent for longer.
By providing the appropriate information to residents and caregivers while also making interventions relevant and fun, will indeed lead to a decrease in falls.
Equipment Considerations?
Some pieces of equipment that could help prevent falls include:
- Hip protectors/Hipsavers
- Head protectors
- Limb protectors
- Sensor alarms in beds and on floors
- Fall out mats
- Concave mattresses
- Bed rails
- Lap belts
Proper footwear is also a big deal when talking about equipment. A shoe is considered safe when the laces are strong, the collar is high and supportive, the heel is low and square, the soles are non-slip, and a thin but firm midsole for the person to “feel” the floor properly.
Observation and Communication?
It’s imperative that in aged care facilities that there is a commitment by everyone to stay alert, observant, and to report any signs that someone might be in danger of falling or of any hazards that could cause someone to fall.
Disease/Medication Review and Risk Management?
By reviewing the diseases and medications that residents are dealing with will be important to managing the risk factors they each carry. From there, specific interventions can be made based on these assessments.
Overall, you can lessen the risk of all the residents in an aged care facility when you expose them to vitamin D, meaning you make sure they get around 20 to 30 minutes of sunlight three times per week. It reduces fracture risk.
Incident Reporting ?
Finally, it’s incredibly important to fill out an incident report when falls do occur. Regardless of where the fall happened or if the person is injured, it’s absolutely necessary to fill out an incident report.
In the report, make sure to note what happened immediately before and during the fall. Details of the fall are then used to create an individualised falls prevention strategy for that resident, hopefully preventing future falls.
In Summary ?
Overall, you might be surprised to know that 30 to 40% of all falls are preventable. Here are some important takeaways:
- Avoid polypharmacy-possible side effects of medication
- Exercise improves balance and muscle strength
- Make environmental modifications when you can
- Be sure that care staff adheres to mobility and toileting orders
- Consider helpful equipment like hip protectors
- Employ behavioural and RAO programs
- Encourage a quick RN response to medical-related falls
- Created detailed incident reports of falls and conduct fall reviews
At Physio Inq, our certified physiotherapists & allied health care professionals are well-versed in the low-impact exercises that help our older generations prevent harmful falls. With the help of our mobile and homecare services, aged care services, occupational therapy services & NDIS services, Physio Inq can help keep you safe and strong no matter how old you are. Give us a call today on 1300 731 733 or find your local Physio Clinic or Home service.
Live a life with less limits.
Date Published: Tuesday, July 9, 2019
Locate a Aged Care Physiotherapy
Service Near me
Get the experience & convinence you deserve to support your or a loved one's allied health needs.
Our Aged Care Physiotherapy team are currently serving & taking appointments in the following states and regions in Australia:
New South Wales
- Blacktown
- Blue Mountains
- Campbelltown And Macarthur
- Canterbury-Bankstown
- Eastern Suburbs Sydney
- Georges River
- Hawkesbury
- Inner East Sydney
- Inner West Sydney
- Lake Macquarie
- Lower North Shore
- Newcastle
- Northern Beaches
- North Sydney
- Parramatta
- Penrith
- Southern Highlands
- South West Sydney
- Sutherland Shire
- Sydney CBD
- The Hills Shire
- Upper North Shore
- Waverley
- Wollongong
Tasmania
Victoria
Need to get into direct contact with ur Client Services team? We're all ears. Call our team directly on 1300 731 733






