Make an Appointment
You may have heard of the chronic muscular condition known as fibromyalgia. While fibromyalgia only affects a small portion of the population (2-5%), it’s common enough to have some name recognition.
Polymyalgia rheumatica, on the other hand, is lesser-known and even rarer (affecting only 0.5% of the population) but shares many similarities to fibromyalgia.
If you’re dealing with muscle pain and you’re not sure why, it’s important to know the difference between fibromyalgia and polymyalgia rheumatica.
So, let’s go over what is the difference between fibromyalgia and polymyalgia rheumatica to give you a better understanding of both.
What is polymyalgia rheumatica?
Polymyalgia rheumatica is an inflammatory form of arthritis that causes muscle pain. Different from fibromyalgia, polymyalgia rheumatica is considered an autoimmune disease which are disorders that cause the body to mistakenly attack healthy tissue.
Polymyalgia rheumatica is rarer than fibromyalgia and occurs most often in older adults over age 65 with the average age of onset being 70 years old.
To diagnose polymyalgia rheumatica, blood tests are usually required since most people with polymyalgia rheumatica have an elevated level of inflammatory proteins in their blood that are easy to detect. Red blood cells in a blood test may also show characteristics of inflammation to help doctors diagnose polymyalgia rheumatica.
Other ways to diagnose polymyalgia rheumatica include imaging tests like X-rays or ultrasound and biopsy tests to check for a related condition known as giant cell arteritis.
Is polymyalgia rheumatica a serious condition?
According to Arthritis Australia, polymyalgia rheumatica is not a serious condition as symptoms usually improve with treatment. Symptoms of polymyalgia rheumatica are even known to lift dramatically within only a few days of the right treatment.
While it can take anywhere between a few months to up to five years for polymyalgia rheumatica to settle itself completely by participating in regular treatment to keep symptoms under control, it’s certainly a manageable condition. However, polymyalgia rheumatica can return if you stop treatment. Still, once you’ve reached remission, it’s rare for it to return.
Another positive is that polymyalgia rheumatica does not cause permanent joint damage. Still, perhaps the most serious form of polymyalgia rheumatica is when it leads to giant cell arteritis. So, if you’re experiencing frequent headaches or loss of vision during your polymyalgia rheumatica treatment, contact your doctor.
So, while polymyalgia rheumatica isn’t serious in and of itself, it should still be taken seriously as its symptoms can certainly have an impact on your everyday life. For example, it’ll likely be difficult to perform daily activities such as:
- Getting out of bed
- Standing up from a chair
- Getting into and out of a car
- Combing your hair
- Bathing and grooming
- Getting dressed
After a while of struggling to do these everyday activities due to your polymyalgia rheumatica, these difficulties can severely affect your mental health, social interactions, physical health, sleep, and overall well-being – all of which are worthy of concern.
Is polymyalgia rheumatica hereditary?
Yes, polymyalgia rheumatica may be hereditary.
While the exact cause of polymyalgia rheumatica is unknown, we know that it is caused by inflammation. What causes the inflammation, however, is still a mystery but there are certain risk factors including heredity.
People of northern European and Scandinavian descent have a higher risk of developing polymyalgia rheumatica than other ethnic groups. Women are also more susceptible meaning that genetics and heredity may play a role in polymyalgia rheumatica.
Other risk factors for polymyalgia rheumatica include:
- Age with the average polymyalgia rheumatica symptoms appearing at age 70
- Environmental exposure as polymyalgia rheumatica cases tend to come in a seasonal pattern which suggests an environmental trigger such as a virus may play a role
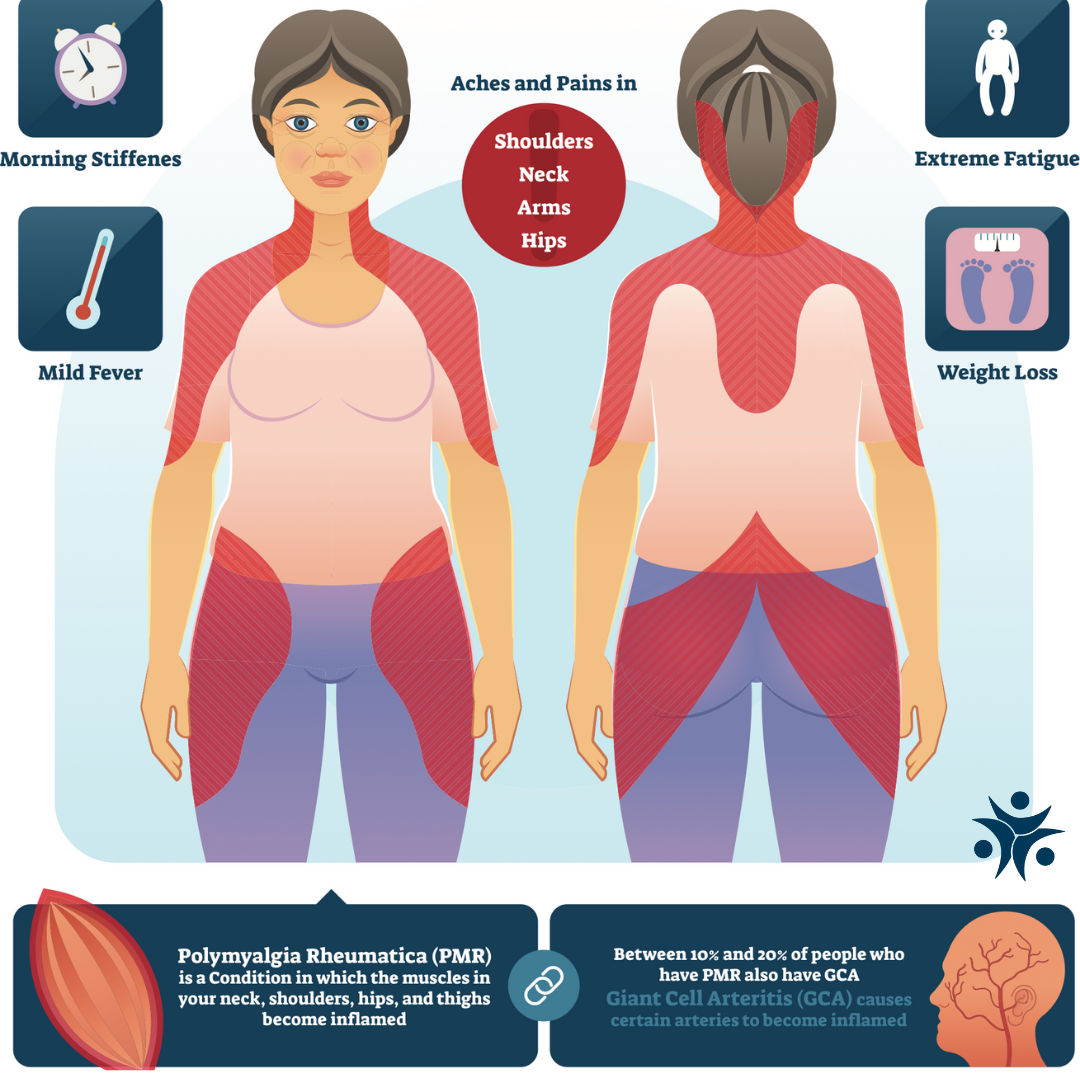
Symptoms of Polymyalgia Rheumatica
Symptoms of polymyalgia rheumatica tend to come on quickly. Sometimes, they can even start overnight. However, symptoms may also develop slowly over time.
Polymyalgia rheumatica causes widespread pain throughout the body. However, some of the major symptoms of polymyalgia rheumatica include:
- Pain and stiffness in the shoulders, neck, upper arms, hips, buttocks, thighs and sometimes in the wrists, elbows, or knees
- The stiffness is almost always worst in the morning when it can severely limit the ability to perform basic tasks, such as getting out of bed and getting dressed
- Fatigue
- Low-grade fever
- Loss of appetite
- Malaise (the general feeling of unwellness)
- Depression
Since there’s also a close link between polymyalgia rheumatica and giant cell arteritis, giant cell arteritis can cause symptoms such as:
- Headache
- Jaw pain
- Vision changes including blurred vision
Up to half of those with giant cell arteritis also have polymyalgia rheumatica while only 10% of those with polymyalgia rheumatica have giant cell arteritis.
Symptoms of polymyalgia rheumatica are like fibromyalgia symptoms in many ways. However, there are similarities and differences between these two conditions including:
- Location of the pain
- Mental health responses
- Morning stiffness
- Sleep problems
Location of the Pain
The location of the pain differs between polymyalgia rheumatica and fibromyalgia.
Those with fibromyalgia experience pain on both sides of the body, usually in 18 main areas. On the other hand, those with polymyalgia rheumatica usually feel pain and stiffness in their shoulders, neck, back and hip girdles.
Mental Health
Fibromyalgia and polymyalgia rheumatica are similar in terms of mental health symptoms as they both may cause depression.
Since it’s tough on anyone’s mental health to live with a painful chronic disease, studies have shown that (especially with fibromyalgia), sufferers have higher rates of PTSD than the average person.
People with both fibromyalgia and polymyalgia rheumatica may also report having trouble focusing and concentrating or a sense of mental fog.
Morning Stiffness
Both fibromyalgia and polymyalgia rheumatica also cause morning stiffness where the muscles and joints feel tight and immobile.
However, morning stiffness tends to persist longer throughout the day if you have fibromyalgia whereas with polymyalgia rheumatica, this stiffness usually only lasts about an hour.
Sleep Problems
Those with both fibromyalgia and polymyalgia rheumatica also often report trouble sleeping which is a secondary symptom caused by the constant pain.
Sleep is incredibly important to overall health and well-being which can cause a ripple effect and make every aspect of life more challenging.
What does polymyalgia pain feel like?
The pain of polymyalgia rheumatica feels like pain and stiffness in the muscles of your shoulders and upper arms as well as in your hips.
The pain is more likely to come on after resting and is usually most severe upon waking from sleep when your muscles and joints have been inactive for an extended period.
What triggers polymyalgia rheumatica?
The trigger for polymyalgia rheumatica is unknown. However, polymyalgia rheumatica is diagnosed
more frequently during certain seasons and in cycles. This suggests that polymyalgia rheumatica may be triggered by something in the environment such as a virus.
Treatment of Polymyalgia Rheumatica
Since polymyalgia rheumatica is caused by inflammation, treatment is focused on reducing inflammation in the body. Treatment for polymyalgia rheumatica, therefore, includes anti-inflammatory steroid medication – the most common and effective being corticosteroids.
While fibromyalgia is like polymyalgia rheumatica, their treatment plans are quite different as fibromyalgia treatment focuses on pain management and reducing central sensitisation. Those with fibromyalgia also tend to focus on making lifestyle changes with exercise and cognitive behavioural therapy to manage symptoms.
Additional treatment options that may help with both polymyalgia rheumatica and fibromyalgia include:
- Acupuncture
- Massage therapy
- Dietary changes towards a more anti-inflammatory diet
- Stress management
- Sleep hygiene
- Avoiding fibromyalgia triggers
- Improving the ease of daily tasks (rolling suitcases, avoiding high heels)
- Calcium and vitamin D supplements to prevent bone loss and steroid side effects
It’s important that polymyalgia rheumatica sufferers stick with their treatments. Otherwise, they won’t work. On the other hand, consistent treatment means those with polymyalgia rheumatica can be symptom-free in a few years.
However, it should be noted that long-term use of corticosteroids as polymyalgia rheumatica anti-inflammatory treatment can have serious side effects including kidney problems, vision changes and high blood pressure.
Keep in mind that if you have polymyalgia rheumatica and are suspicious that you might also have giant cell arteritis, see a doctor right away for more specialised treatment.
What is the best pain relief for polymyalgia?
The best pain relief for polymyalgia rheumatica is corticosteroids. These injections offer both pain relief and anti-inflammatory benefits which are incredibly effective at treating polymyalgia rheumatica symptoms.
In fact, corticosteroids have proven to be so effective for polymyalgia rheumatica that if they don’t offer you relief, polymyalgia rheumatica may be a misdiagnosis.
While you might assume that non-steroidal anti-inflammatories (NSAIDs) would also be effective pain relief for polymyalgia rheumatica, this is unfortunately not the case. Without a doubt, corticosteroids are the best pain relief for polymyalgia rheumatica.
Living with Polymyalgia Rheumatica
Living with polymyalgia rheumatica is often incredibly stressful and can leave people feeling depressed about their situation. However, with the right treatment plan and lifestyle changes, polymyalgia rheumatica doesn’t have to be a serious hindrance to your life.
Plus, the good news is that, unlike fibromyalgia, polymyalgia rheumatica isn’t a chronic disease and can be sent into remission over the course of a few years.
Living well with polymyalgia rheumatica includes:
- Eating a more anti-inflammatory diet
- Stress management techniques like meditation and regular exercise
- Sleep hygiene such as starting an evening routine
- Improving the ease of daily tasks by using rolling suitcases and avoiding high heels
To learn more about polymyalgia rheumatica and find ways you can better manage your symptoms, check out Arthritis Australia or speak to one of our expert physiotherapists at Physio Inq today!

Date Published: Tuesday, April 26, 2022
Locate a Mobile Physiotherapy
Service Near me
Get the experience & convinence you deserve to support your or a loved one's allied health needs.
Our Mobile Physiotherapy team are currently serving & taking appointments in the following states and regions in Australia:
New South Wales
- Blacktown
- Blue Mountains
- Campbelltown And Macarthur
- Canterbury-Bankstown
- Eastern Suburbs Sydney
- Georges River
- Hawkesbury
- Inner East Sydney
- Inner West Sydney
- Lake Macquarie
- Lower North Shore
- Newcastle
- Northern Beaches
- North Sydney
- Parramatta
- Penrith
- Southern Highlands
- South West Sydney
- Sutherland Shire
- Sydney CBD
- The Hills Shire
- Upper North Shore
- Waverley
- Wollongong
Tasmania
Victoria
Need to get into direct contact with ur Client Services team? We're all ears. Call our team directly on 1300 731 733














